Abstract
Background:
In patients with diffuse large B-cell lymphoma (DLBCL), adequate follow-up is required with the improvement of prognosis. The efficacy of scheduled imaging for patients with DLBCL who achieved complete response (CR) is discussed. The possibility to avoid surveillance imaging have been reported, although most studies are based on a small number of cases. The NCCN guideline version 4.2018 recommend not to perform scheduled imaging routinely for follow-up, or only for patients with stage III/IV. However, there is no strong evidence of supporting the inferiority of scheduled imaging. It is possible that some patients might benefit from scheduled imaging.
Methods:
We investigated patients with de novo DLBCL who were diagnosed in The Cancer Institute Hospital of Japanese Foundation for Cancer Research, Japan from 5 January 2013 to 31 May 2016 retrospectively, to conduct a sampling of first relapsed patients after CR. Patients who achieved CR after salvage therapies were included. Patients who received first-line therapy without rituximab because of non-approved use at the time were excluded. Relapse diagnosis without pathological proof were permitted. Eligible patients had a minimum of 2 years follow-up. All data were updated 17 July 2018. Overall survival (OS) was censored at the last date of follow-up.
Relapsed patients were divided into 2 groups according to a momentum of diagnosis, clinical symptoms (symptom group) or scheduled imaging (imaging group). Clinical symptoms are defined as subjective complaint, physical exam finding and blood test abnormality. Imaging modality includes echography, computed tomography (CT), magnetic resonance imaging and positron emission tomography/CT. The Hans classifier, using CD10, BCL6, and MUM1 immunohistochemistry, was used to categorize as germinal center B-cell-like (GCB) or non-GCB.
Fischer's test was used for comparative between the symptom group and imaging group, Kaplan-Meier test for calculate survivals, the logrank test for statistical analysis of OS, event-free survival (EFS) and survival parameters. All statistical analyses were performed with EZR software.
Results:
A total of 759 patients were identified as de novo DLBCL. Then 630 achieved CR, 527 had maintained CR and 103 relapsed. Among the 103 cases, 7 patients were excluded because of lack of some data. Eventually, 96 patients with first relapse were enrolled in this analysis. Relapse was confirmed pathologically in 85% (82/96) cases. Only in the symptom group, all 7 cases were not received biopsy because of central nervous system involvement. Most patients were scheduled to perform imaging every 6 months.
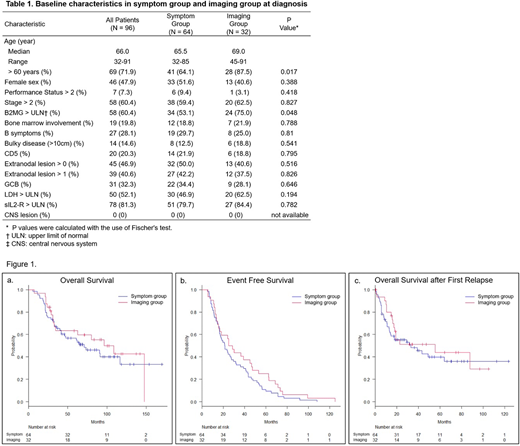
We divided the 96 first relapsed patients into 2 groups by the momentum of relapse diagnosis. The median follow-up duration was 56.1 months. While 67% were detected by clinical symptoms, 33% had relapse diagnosis by scheduled imaging, and their characteristics are summarized in Table 1.
Significant differences in the outcome were not found between the symptom group and the imaging group: 4-year OS (57%, 95% confidence interval [CI] 0.44-0.68 vs. 4-year OS: 63%, 95% CI 0.44-0.78; P = 0.517), 4-year EFS (20%, 95% CI 0.12-0.31 vs. 28%, 95% CI 0.14-0.44; P = 0.163), and median OS after first relapse (33.0 months vs. 55.4 months; P = 0.512), respectively (Fig 1).
In the symptom group, indications were lymph node swelling (38%), neurological symptoms (20%), subcutaneous mass (17%), head and neck discomfort (10%), B symptom (6%) and blood test abnormality (3%). Univariate analysis revealed that only the existence of B symptoms at first diagnosis was significant for OS (P = 0.0361). Multivariate analysis using stepwise multiple logistic regression also demonstrated that the existence of B symptoms at first diagnosis to be the single independent factor of OS (P = 0.0402). In the imaging group, univariate analysis revealed that the existence of B symptoms at first diagnosis was significant for OS (P = 0.0241). There was no significant difference in OS between patients with stage I/II and stage III/IV in the 96 relapsed patients (P = 0.618).
Conclusion:
These results indicate that routine image surveillance in DLBCL patients during their first CR does not improve OS and EFS. However, B symptoms at first diagnosis was a significant factor for OS in both the symptom and imaging group, Patients with B symptoms at diagnosis might receive a benefit of image surveillance.
Nishimura:Chugai pharmaceutical inc, Roche: Other: commissioned work. Mishima:Chugai pharmaceutical inc, Roche: Other: commissioned work. Yokoyama:Chugai pharmaceutical inc, Roche: Other: commissioned work. Terui:Celgene: Honoraria; Bristol myers Squib: Honoraria; Janssen Pharmaceutical KK: Honoraria; Takeda pharmaceutical: Honoraria; Novartis pharma: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal